Pelvic floor disorders are a set of disorders related to the woman’s pelvis and the pelvic floor, and to the different organs and support systems in that area, (muscles, ligaments, fasciae, etc.). Weakness of or injury to the various support systems or pelvic organs, may affect the normal function of surrounding organs, such as the bladder, urethra, vagina, uterus, vulva and rectum. Women with PFDs may experience various symptoms:
- Urinary problems, such as urinary incontinence, mainly following a stressful event (stress urinary Incontinence, SUI) but also an urgent need to urinate, urge incontinence, painful urination, incomplete emptying of their bladder, etc.
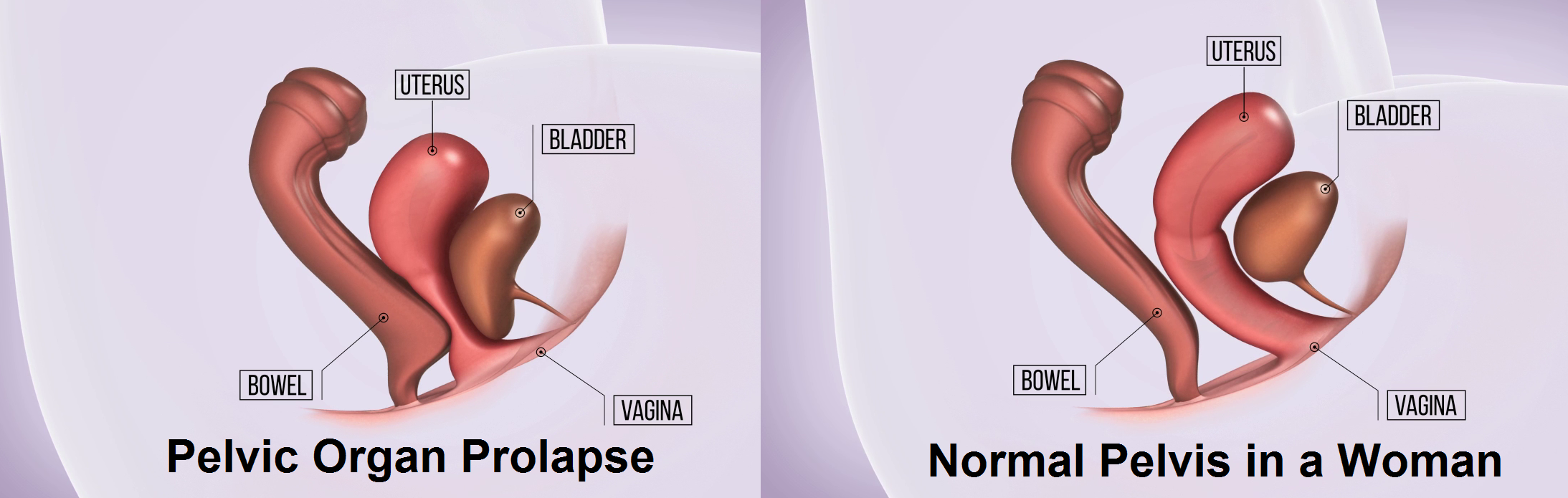
- Pelvic organ prolapse – where weakness of the pelvic support system causes various surrounding organs to prolapse into the vaginal cavity with various resultant complaints
- Rectal problems such as fecal incontinence, constipation, straining or pain during bowel movements.
- Sexual dysfunction
- Pain or pressure in the vagina or rectum.
- Other less frequent complaints
The most prevalent PFDs are urinary incontinence and pelvic organ prolapse which affect around 50% of the female population, worldwide, and are associated with huge financial burden on both patients and medical systems.